Why Did Ultrasounds Become Routine?
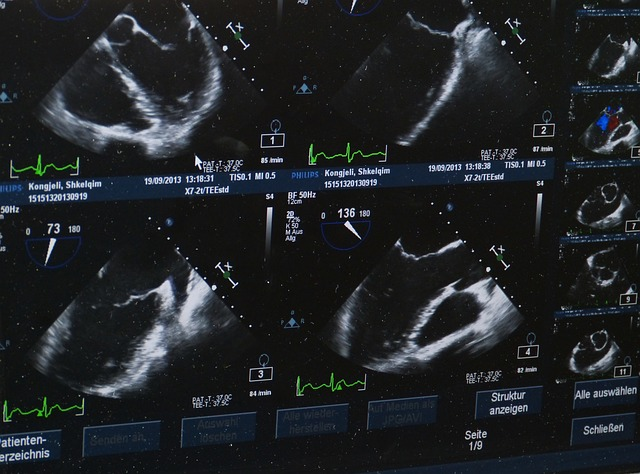
Today's children have been exposed to an unprecedented level of ultrasound technology, both in frequency and intensity. In 2001, 67% of pregnant women had at least 1 ultrasound, and in 2009, that percentage jumped to 99.8% with an average of 3 per woman. What accounts for this increase? Do we have evidence to suggest that this intervention is saving lives, changing outcomes, and that it is safe? What about safety in the settings it is applied most frequently, such as advanced maternal age, metabolic syndromes, and complications? Could these higher risk pregnancies represent a category of fetus that is more vulnerable to potential side effects of an intervention like ultrasound?
It appears that, answers to these questions remain elusive despite widespread application for the following conventionally accepted reasons:
- Gender determination
- Screening for anomalies
- Assessment of size/fluid level
- Visualization for bonding/curiosity/entertainment
- Assessment of placental position
As one survey concluded,
"Women appear to want sonograms for reasons that may not assist their provider with immediate clinical decision making. This is a potentially important disagreement between cost-saving and patient satisfaction that maternity care providers must consider when deciding whether to perform prenatal sonography for women with low-risk pregnancies."
In other words, women are lured into the prospect of reassurance and information about an uncertainty-laden bodily experience, and providers may cater to that desire in neglect of accumulating concerns, lack of benefit, and conflict around financial gains ($86-102/scan).
Are They Safe and Effective?
As is the case for most habitual rather than evidence-based medicine, the vast majority of women undergoing this procedure are not adequately consented about the potential ultrasound risks and the state of benefits as acknowledged by objective assessment of the literature.
Assumptions about the technology's safety allowed it to be grandfathered in to FDA clearance in 1976.
Epidemiologic studies of ultrasound safety were conducted before 1992, and would have been representative of significantly less cumulative epigenetic burden to the fetus, as they predated changes to the childhood vaccination program and the flooding of our diets with genetically modified foods – all of which may synergize in a vulnerable child to contribute to chronic neurodevelopmental problems.
In the past several decades, ultrasound technology has evolved in terms of peak exposure and intensity (from 46 to 720 mW/cm2), and newer versions remain largely unstudied.
McClintic et al's results corroborate existing findings that evidence concern for delayed learning and reduced hippocampal neuronal dopamine, norepinephrine, and serotonin, as well as disrupted neuronal migration, a defect implicated in the pathogenesis of autism. Investigative journalist Dr. Jennifer Margulis has documented research including interviews with Dr. Manuel Casanova, a neurologist and neuroscience researcher, who discusses characteristic changes in gestational brain development in autistic children that can be produced by ultrasound exposure, as well as the epidemiologic overlap between escalating ultrasound exposure and autism incidence.
Randomized studies in humans point to potential increased incidence of low birth weight, delayed speech, poor school performance, dyslexia, and non-righthandedness.
Safety studies, even if they were undertaken in a placebo-controlled manner, rarely are longitudinal enough to account for neurodevelopmental delay declaring itself later in childhood.
McClintic et al hypothesize that acoustic radiation, which may impact brain action potentials through calcium signaling, may be the mechanism by which ultrasound impacts neurodevelopment, when it does. Other putative impacts are cavitation and heating, which is particularly relevant with non-pulsed Doppler technology. According to the peer-reviewed medical resource, UpToDate:
Spectral Doppler ultrasound, however, uses higher energy and focuses the acoustic energy that is created on a much smaller volume of tissue than typical 2D imaging does, and can result in changes in tissue temperature, especially at bone-tissue interfaces. For this reason, Doppler ultrasound should be used with great care, especially early in pregnancy.
With regard to "efficacy," multiple Cochrane reviews have demonstrated a lack of perinatal mortality benefit for routine ultrasound in a normal pregnancy, and an increased risk of cesarean section with third trimester screening. A review of outcomes literature condemns ultrasound when used for dating, second trimester organ scan, biophysical profile, amniotic fluid assessment, and Doppler velocity in high and low risk pregnancies. We want to believe that this intervention is changing the health of pregnancies, but that is not what has been demonstrated. Ultrasound may have a limited role in detection of a treatable (often with 50% mortality risk) indication, which Judy Cohain CNM states only includes spina bifida, diaphragmatic anomaly, twin-twin transfusion syndrome, bladder obstructions, and sacrococcygeal tumor. False positive rates are significant on routine scan, and anxiety-provoking at best, and at worst, result in terminations for anomalies less severe than perceived by ultrasound as was the case in 1 in 200 ultrasound-influenced abortions.
For these reasons, routine prenatal ultrasound is not recommended by the American College of Obstetrics and Gynecology, for non-medical use and UpToDate states,
The primary objective is to obtain information that will enable delivery of optimal antenatal care and thus the best possible outcomes for mother and fetus. However, the benefit of such prenatal sonographic screening on neonatal outcomes remains unproven.
So Why is Every Woman Walking into an OBs Office Getting Probed With a Jelly-Slicked Wand?
It is because habit, profit, and community consensus are driving your care, not evidence or the precautionary principal. In fact, in this review, of 717 obstetrical recommendations, only 30% reflected good quality evidence. That leaves you, the patient to make your own decisions about health care interventions.
Is it possible to fly blind throughout a pregnancy, without a cute little profile pic or scrunched claymation images of your little bundle-to-be?
It is, and this is an option worth considering. Each and every recommended ultrasound should be thoughtfully pursued in light of unanswered questions and growing concern. Avoiding ultrasounds is a gift to your mental health in that it may just liberate you to experience the pregnancy for what it is, rather than to jump from one externalized nail-biting milestone to another.
Pregnancies, cared for by thoughtful women and their loved ones are marked by maximizing health through a low glycemic, high natural fat diet, exercise, relaxation response, and careful environmental detox of plastics, pesticides, air and water contamination, and genetically modified foods. Preparing for pregnancy in advance of conception, through these measures, is the best reassurance of fetal health available. When we step back and allow for the complexity of gestation to unfold unhindered, we may recognize the danger in micro management of a normal physiologic pregnancy and birth experience.
Dr. Brogan is boarded in Psychiatry/Psychosomatic Medicine/Reproductive Psychiatry and Integrative Holistic Medicine, and practices Functional Medicine, a root-cause approach to illness as a manifestation of multiple-interrelated systems. After studying Cognitive Neuroscience at M.I.T., and receiving her M.D. from Cornell University, she completed her residency and fellowship at Bellevue/NYU. She is one of the nation’s only physicians with perinatal psychiatric training who takes a holistic evidence-based approach in the care of patients with a focus on environmental medicine and nutrition. She is also a mom of two, and an active supporter of women's birth experience. She is the Medical Director for Fearless Parent, and an advisory board member for GreenMedInfo.com. Visit her website.
Disclaimer: This article is not intended to provide medical advice, diagnosis or treatment. Views expressed here do not necessarily reflect those of GreenMedInfo or its staff.
Internal Site Commenting is limited to members.
Disqus commenting is available to everyone.
This article is copyrighted by GreenMedInfo LLC, 2014
Visit our Re-post guidelines
How to Share GreenMedInfo.com Content
This work may be reproduced and redistributed, in whole or in part, without alteration and without prior written permission, provided all copies contain the following:
1. "© [Article Date] GreenMedInfo LLC. This work is reproduced and distributed with the permission of GreenMedInfo LLC. Want to learn more from GreenMedInfo? Sign up for the newsletter here http://www.greenmedinfo.com/greenmed/newsletter."
2. Complete original title and author credit directly below the headline.
3. An original do-follow hyperlinks intact and active going back to the article location you are reproducing; all other hyperlinks within the article are do-follow and remain intact.
4. No changes or edits to title, content, hyperlinks, or images are permissible without written permission from GreenMedInfo LLC.
If you have questions or need further information, please contact kate@greenmedinfo.com.
_______________________________________________________
PLEASE DONATE TODAY, IF the Holy Spirit impresses you, (donate button below and on the side) so I can continue to help others. Thank you! If you can't see the donate button or want quick access – use this link: PayPal.Me/ReneeB
Got info from another source.
No comments:
Post a Comment